The opening two lines of the preamble of the WHO Constitution read:
- "Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity."
- "The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition."
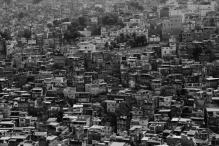
The right to health is not only enshrined within the preamble of the WHO Constitution, but exists in international human rights treaties, regional instruments, and over 100 constitutions around the world. However, even prior to the pandemic and the events of the last two years, it was already abundantly clear that the rhetoric of a right to health did not match up to reality. It was not serving those most in need within countries at the local level, nor was it being fully addressed by the primary global health institutions (e.g. WHO, UNICEF, and others) with the responsibility for upholding rights and health in their mandates.
A closer look highlights an interplay of factors contributing to this. First, the impact of economic, social, cultural and political forces on the normative and operational aspects of both health and human rights locally and globally; second, the impact of national ideologies on geopolitical conversations and the consequences on our (in)ability to assert human rights in health or health in human rights; third, the limited investment, interest, and capacity within global health institutions to incorporate human rights in their work; and lastly, the severe limitations of the present architecture which is inapt to sufficiently address current realities (e.g. issues that transcend border like climate or the power of corporate actors) appearing to address global and national development priorities.
Health is political. And even as rights are meant to transcend politics, the erosion of rights protections in the name of public health is not new and it is nothing if not political. Reaffirming health as a human right would therefore entail as a first step remembering, adjusting, and building on the institutions, norms and standards which are foundational. The drafters of the WHO Constitution were clear on the need to recognise and address inequalities and ensure human rights as cardinal to health. Pandemics, climate change and conflict have all exposed deep fissures not only in our understanding, but in our application of these concepts to health and well-being.
We always need to do more to address who gets sick and why, who gets left behind and why, whose health needs are provided for and whose are not, and what it will take to maximise the role that systems of governance and accountability play in ensuring health for all. Addressing these questions is still vitally needed, and lies at the heart of making health as a human right real.
Science matters, but all science and not just biomedical interventions
The global health discourse continues to be dominated by biomedical sciences, and far too little attention is given to the contribution and role of other relevant sciences to health and well-being. The events of the last two years have demonstrated nothing, if not the importance of embedding political science, anthropology, and social sciences into the core of health research, policymaking, and programming. Yet, despite the rhetoric, funding streams largely continue to ignore all but the biomedical. One simple example, the former head of the US National Institutes of Health (NIH) Francis Collins in stepping down noted that the insights of social science to address vaccine hesitancy were badly needed, even as he recognised that the NIH had not prioritised funding for this area of research.
Neglecting the role and contribution of sciences other than biomedical has created a paradox. On the one hand, global health institutions are increasing their rhetoric with regard to addressing human rights, inequities, gender inequalities, and other determinants of health. On the other, programming and investments remain predominantly focused on biomedical interventions and programmes. Not only recognising but financing the critical role of diverse scholarship and epistemologies and ensuring integrated research, policymaking, and programming are key to enhancing the effectiveness and sustainability of interventions for peoples health and well-being.
It’s all about context: context is everything
The variability and specificity of contexts and their bearing on what will be most effective in health policymaking and programming are critical. Far too often, overly generalised approaches are adopted resulting in the development of guidelines, policies, and programming by national governments and global health institutions, with limited concrete attention to how variability of contexts and local dynamics will impact the feasibility of implementation. Not surprisingly, often resulting in limited uptake, outright rejection or adoption in ways that may not be relevant and therefore largely ineffective.
It is worth investigating the impacts of the adoption of countless guidelines promulgated by WHO and other global health institutions, which, even when scientifically sound and evidence-based, often lack efforts to address context-specific knowledge. Evidence is clear from across a spectrum of health issues — from vaccines to sexual and reproductive health, to child health to WASH (water, sanitation and hygiene) — that economic, social, cultural, political and legal contexts matter and where such context is not siloed but factored in, the potential success of interventions grows exponentially.
Politics of data
In global health, one still hears the metaphor, ‘what gets measured, gets done’. Increasingly, it is proven that the converse of this is what is actually true: ‘what gets measured is what we want to get done’. The questions then are who is the ‘we’ doing the measuring, why a particular focus, what is counted, what is not, and why. There are many blind spots in the who, where, what, and why of how data are collected and interpreted, even when they set out to address what would seem to be topics lending themselves directly to a right to health analysis such as gender inequality in access and outcomes (e.g. in the context of COVID-19, Ebola or, for that matter, health research overall), certain health topics (e.g., abortion) or the intersection of health with inequalities more broadly.
Ironically on each of these topics, validated indicators and methodologies for collecting data exist, even as they are not often used, besides some boutique level projects. This of course raises the question: if such data are not collected in those health areas where relevant indicators already exist, and when collected are not part of determining priorities, what does this mean for attention to these issues in global health more broadly? Unfortunately, the answer is all too clear: those in positions of power often prioritise indicators where the data are easy to collect and consistent with current funding strategies, resulting in inattention to issues that cannot easily be addressed or that they do not want to address. Despite a global commitment to leaving no one behind, the lack of relevant indicators and consequently of relevant data, results in ongoing systematic disenfranchisement and poor health outcomes for key population groups across the globe.
Gender equality is necessary for health as a human right
Attention to gender in all its manifestations and diversities is fundamental to health as a human right. However, gender and other intersecting inequalities, including race and class, continue to be a casualty of global health discourse. Much of public health research is and continues to be modelled on the health specificities of an idea of ‘normal’ defined through the narrow lens of a prevailing orthodoxy. Sex and gender diversity, for example, are held ransom to the notion of ‘normal’; a situation that further perpetuates inequalities, inequity, injustice and rights violations. Understanding these challenges lies at the centre of defining and achieving success in programming, policymaking, and effective implementation.
Laws matter as much as medicine
The preface of the 2012 Global Commission on HIV and Law report reads, "Law prohibits or permits specific behaviours, and in so doing, it shapes politics, economics and society". The Law can be a human good that makes a material difference in people’s lives. Therefore, it is not surprising that law has the power to bridge the gap between vulnerability and resilience to HIV.
As the events of the last two years (and much before) showcased, the importance of legal environments in shaping health outcomes is relevant for many areas of global health. Whether it was overzealous restrictions during the lockdowns which resulted in abuses of human rights and negative impacts particularly on the health of the most poor and marginalised the world over; or undue restrictions on access to services deemed not essential by those in power for some but not all populations, recent experiences underscore the ways in which law and its implementation play a cardinal role in global health.
However, far too often, inadequate attention is paid to legislative aspects resulting in lacunae whereby even the best health interventions are not nearly as effective as they could be — whether because of the existence of explicitly restrictive legislation impacting their reach to the populations who need them most or the absence of an enabling and supportive legal environment more broadly.
Capacity and willingness of states and other institutions of power
The last two years have highlighted the many ways States are incapable or unwilling to implement the measures related to global health that will help those most in need, within their borders and beyond. This can result not only from unwillingness, but also from a lack of capacity, both highlighting the need for steady, reliable and depoliticised international assistance and cooperation. Within the context of the pandemic, WHO recognised this early on and noted: "LMICs will require international assistance and cooperation to fully manage the impact of COVID-19 on their populations. Under international human rights law, the obligations undertaken by State parties beyond their borders, (i.e. to International Assistance and Cooperation) are akin to their domestic obligations, not subsidiary or secondary in any way. COVID-19 is a reminder, not only of the global connectedness of solutions."
Beyond just the context of the pandemic, conflict, and climate, it is abundantly clear that significant and sustained investments are required to enhance the capacity of the world at large to respond to global health challenges. In this respect, there is a need for much greater attention to what States say they will do in global spaces and what they actually do in practice. The system is only as strong as the extent to which States live up to their commitments. The great difference between government incapacity and government unwillingness is central here not only for advocacy but for accountability and for ensuring the implementation of measures best suited to the health of all populations, not only those easiest to reach.
Critically also, one must recognise the increasingly oversized role of multinational corporate actors, including but not limited to the pharmaceutical industry, with direct impacts on the health of populations but crucially also on the capacity/willingness of States to respond. Throughout the last two years, we have witnessed the might and greed of corporations — whether the ongoing blocking of patent waivers by pharmaceutical companies despite a raging pandemic or the perpetual actions of the fossil fuel industry or the businesses run by oligarchs and their role in conflicts. The lack of effective means and regulation of these actors for the very real human rights abuses they perpetrate is far too real. The limits of the existing human rights machinery for addressing the harms caused by these types of actors needs not only to be called out but addressed, with explicit attention to what these realities may mean for accountability and for the broader reshaping of global norms, standards and governance.
What about the structures: the need for a global health architecture overhaul?
Writing in the context of the Ukraine Crisis, Richard Gowan commented, "The UN is another casualty of Russia’s war". The Ukraine/Russia conflict has challenged the very foundations on which the United Nations is built, including its mechanisms and processes, a crisis already underway. The WHO and its leadership have come under severe attack for their handling of Ebola, to say nothing of the COVID-19 crisis. The failures of COP26 in Glasgow led one leader to exclaim, 'when would the leaders lead?'. The UN's High Commissioner for Human Rights and human rights mechanisms have been under severe attack for their handling of country situations like China among others. The challenges facing these institutions are enormous, even as the dysfunctionality that plagues them is pervasive and entrenched.
In our 2020 reflections we noted, "the system also struggles with structural weaknesses, block politics and a voting structure which privileges certain countries over others. Member states can rightly be criticised for reducing the UN to a fig leaf that they hide behind, but also a whipping mule". Unfortunately, the two years that have followed prove this further.
It is sadly important, therefore, to restate: "The need for an in-depth review of these institutions today is more acute than ever because the way we strengthen and reshape them will not only determine our collective future but that of generations to come. For any such review to be genuinely transformative, however, it must start with reviewing the member states and their conduct domestically and within these institutions". It is not the drafting of new conventions or treaties that rely on the existing order that will chart the way for a better future, but a deeper introspection and a collective willingness to address the challenges to our common future together.
Recently, the WHO Intergovernmental Negotiating Body has started discussions to draft and negotiate a WHO convention, agreement, or other international instrument, on pandemic prevention, preparedness and response. As a global society that continues to live under the onslaught of the COVID-19 pandemic, it is important that discussions on this new treaty, which remains based in existing structures is not seen as a panacea or sufficient. To be effective, there must not only be good language but an assessment of gaps and lacunae within existing norms and standards, including the International Health Regulations and international human rights instruments, as well as a determination of what it will take to strengthen the systems, approaches and accountability mechanisms needed for their monitoring.
True assessment of the failures in preventing exacerbation of the COVID-19 pandemic and lessons learned has not yet been done. To do so would seem critical to the success of any such process, ideally undertaken as part of a comprehensive review and overhaul of global health, law, human rights, governance, and architecture.
Conclusion
The need and imperative to rethink and reimagine human rights in global health is clear. We catalogue here learnings not only from the past two years but from the last two decades on what will it entail to make health as a human right real. Human rights are not a panacea nor do they guarantee a preordained result, but they are an important tool to ensure health is seen and realised as a global good not only for some but for all. For this to move from rhetoric to reality will require not only addressing the normative, structural and contextual issues we identify here but a new social contract. A contract underpinned by an ethos of human rights, solidarity, and cooperation locally and globally requires mutual accountability, not just promises of good governance and voluntary agreements. The challenges that confront our common future are enormous. Key to addressing them effectively is to reaffirm human rights as our common value, and ensure a global health architecture that is truly ‘fit for purpose’.
•••
This article is republished under a Creative Commons Attribution-NonCommercial 4.0 International license. Read the original article on the BMJ Global Health website.
Suggested citation: Pascale Allotey, Sofia Gruskin and Rajat Khosla. "Reimagining Human Rights in Global Health: What Will it Take?," United Nations University, UNU Centre, UNU-IIGH, 2022-10-04, https://unu.edu/article/reimagining-human-rights-global-health-what-will-it-take.